Jessica Quiles
MBA, BSN, RN, CCRN
Critical Care Registered Nurse with over 5 years of frontline experience delivering complex, high-acuity care across multi-specialty intensive care units and emergency settings. Proficient in ventilator management, invasive hemodynamic monitoring, and titration of advanced vasoactive infusions, with a proven track record of clinical excellence under pressure. A passionate advocate for patient-centered care, I am deeply committed to advancing anesthesia practice as a future CRNA — driven by a mission to improve outcomes for vulnerable and underserved populations, both locally and abroad. My career has been defined not only by clinical expertise but also by leadership, collaboration, and a dedication to lifelong learning. I continually pursue advanced education, specialty certifications, and evidence-based practices to ensure every patient receives the safest, most equitable, and highest quality care possible.
PROFESSIONAL EXPERIENCE
RIVERSIDE MEDICAL CENTER (IL): Emergency Department and Intensive Care Unit RN
September 2022 - Present
Returned on an internal contract to provide patient care in both the Emergency Department and Intensive Care Unit, addressing critical staffing needs.
Stabilize acutely ill and emergent patients, delivering high-acuity critical care interventions in fast-paced, high-pressure environments.
Collaborate with multidisciplinary teams to ensure seamless transitions of care from the emergency department to critical care units, prioritizing patient safety and continuity.
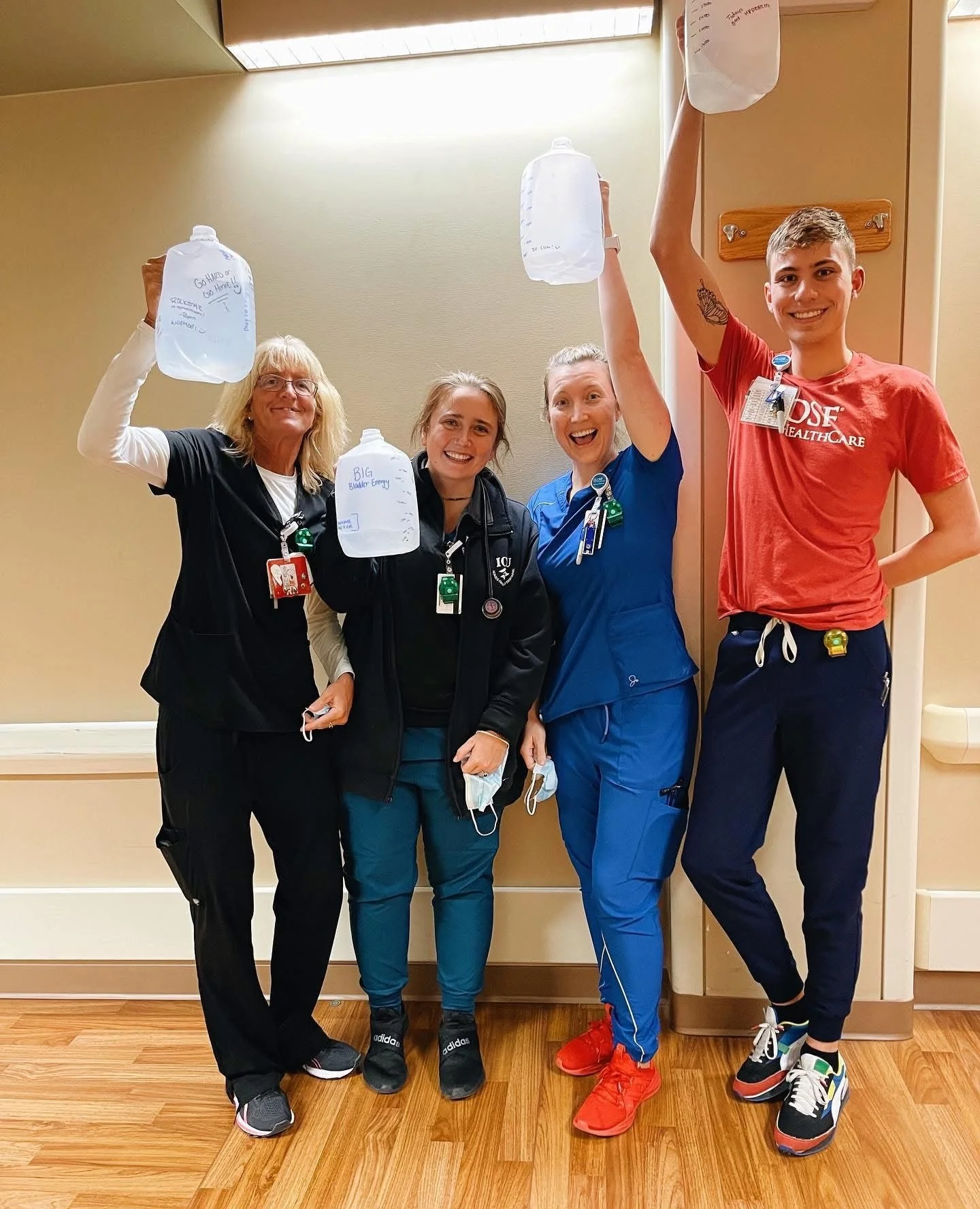
OSF ST. FRANCIS (IL): Float Intensive Care Unit Registered Nurse
September 2021 - September 2022
Delivered comprehensive critical care across multiple ICU specialties, including trauma, surgical, neurological, cardiac, and medical, adapting rapidly to diverse patient populations and clinical workflows.
Managed mechanical ventilation, invasive hemodynamic monitoring, and titration of complex vasoactive medications with precision and adherence to evidence-based practices.
Partnered with rotating teams of physicians and allied health professionals, demonstrating resilience, adaptability, and strong interdisciplinary communication in high-acuity environments.
RIVERSIDE MEDICAL CENTER (IL): Intensive Care Unit Registered Nurse
March 2020 – September 2021
Managed critically ill patients in a combined ICU setting, delivering care across surgical, medical, neurological, and cardiac populations.
Responded promptly to patient deterioration, executing evidence-based interventions and collaborating closely with multidisciplinary teams to optimize outcomes.
EDUCATION
Waubonsee Community College (IL) August 2025 – Present
Pursuing Spanish fluency to improve communication and provide more inclusive care for future patients.
Enrolled in advanced chemistry courses to strengthen foundational knowledge in preparation for CRNA school.
Olivet Nazarene University (IL) March 2022 – March 2023
Master of Business Administration (Healthcare Concentration)
Gained insight into healthcare infrastructure, operations, and business strategy.
Explored healthcare delivery in rural America, with coursework focused on building sustainable facilities to support underserved populations.
Completed a project on mobile healthcare delivery models, emphasizing access, efficiency, and equity in patient care.
Applied business acumen to clinical practice, fostering a heightened awareness of healthcare resource utilization and waste reduction while maintaining exceptional patient care.
Olivet Nazarene University (IL) August 2015 – December 2019
Bachelor of Science in Nursing
Built a strong foundation in core nursing practice, clinical decision-making, and evidence-based care.
Completed advanced sociology coursework to deepen understanding of human behavior, culture, and the social factors influencing patient health and care delivery.
Growth in Action - Preparing for CRNA School
-

Shadowing CRNA's: Embracing the Full Scope of Anesthesia
Shadowing CRNAs has given me a deeper appreciation for the full scope of anesthesia care. I’ve watched awake patients undergo surgery with regional anesthesia, where the CRNA balances comfort and reassurance, and I’ve seen patients under general anesthesia, medically paralyzed and completely dependent on the CRNA for every breath.
What I love is how CRNAs manage the entirety of the patient—airway, physiology, comfort, and safety—through every phase of surgery. Observing this has not only strengthened my understanding of anesthesia but is also developing my judgment, curiosity, and respect for the role.
Each shadowing experience prepares me more for CRNA school and reminds me why I feel called to step into this profession.
-

Coursework and Certifications
Earning my ACLS, BLS, PALS, and CCRN certifications has strengthened both my clinical skills and my ability to respond under pressure. Preparing now for the CMC and CSC has pushed me to think even more critically about advanced cardiac physiology and hemodynamic management. Alongside these certifications, I have pursued advanced chemistry courses to build a stronger scientific foundation for the rigor of anesthesia school.
I am also studying Spanish with the goal of becoming fluent, so I can better serve vulnerable and underserved communities. Together, these experiences are not only sharpening my knowledge and discipline but also preparing me to care for patients with both excellence and compassion as I move forward toward becoming a CRNA.
I actively read AANA Journal articles and maintain a personal log of clinical takeaways to stay current with emerging research and best practices in nurse anesthesia. This ongoing self-study reflects my commitment to academic excellence and readiness for the rigor of graduate-level anesthesia education.
-

Leadership & Mentorship
Serving as a nurse preceptor for new hires and nursing students has been one of the most meaningful parts of my nursing journey. In this role, I’ve had the privilege of guiding others through the transition from theory to practice. Teaching them how to interpret patient assessments, manage critical situations, and apply evidence-based care at the bedside. Precepting has required me to not only share knowledge but also model confidence, calmness, and critical thinking in high-stakes moments.
What I’ve discovered is that teaching others strengthens my own practice. Explaining pathophysiology, reviewing medication choices, and walking through complex clinical decisions has deepened my understanding while sharpening my ability to think clearly and communicate under pressure. It has also shown me the value of adaptability. Meeting each learner where they are, just as CRNAs must meet each patient where they are in their vulnerability.
Precepting mirrors many of the qualities essential in anesthesia: vigilance, clinical judgment, and the ability to remain steady while leading others through uncertainty. It has reinforced my desire to advance my practice, step into greater responsibility, and carry these same qualities forward as a CRNA.
“Beyond the Bedside”
Volunteering has always been a core part of who I am. It allows me to stay connected to my community beyond the hospital walls. Whether I’m mentoring new nurses, guiding college students, or supporting local outreach efforts, I find purpose in helping others grow and feel supported. Service, to me, isn’t just about giving back—it’s about showing up consistently, sharing knowledge, and creating a ripple effect of positive impact wherever I can.
I’ve had the privilege of volunteering at a low-income, predominantly minority high school, speaking to prospective nursing students about careers in healthcare. These sessions are more than just educational—they’re about planting seeds of confidence and possibility in students who may not have role models in the field. Helping them see a future for themselves in nursing is one of the most rewarding parts of my work.
That sense of purpose deepened even further during a medical mission trip to Africa, where I volunteered at a rural clinic. Working alongside local healthcare providers to care for patients with limited resources reminded me of why I chose this path in the first place. It was a powerful, humbling experience that renewed my commitment to equitable care and strengthened my resolve to serve with compassion no matter where I am in the world.
My Stories — My Truth